Hap Prior Authorization Form
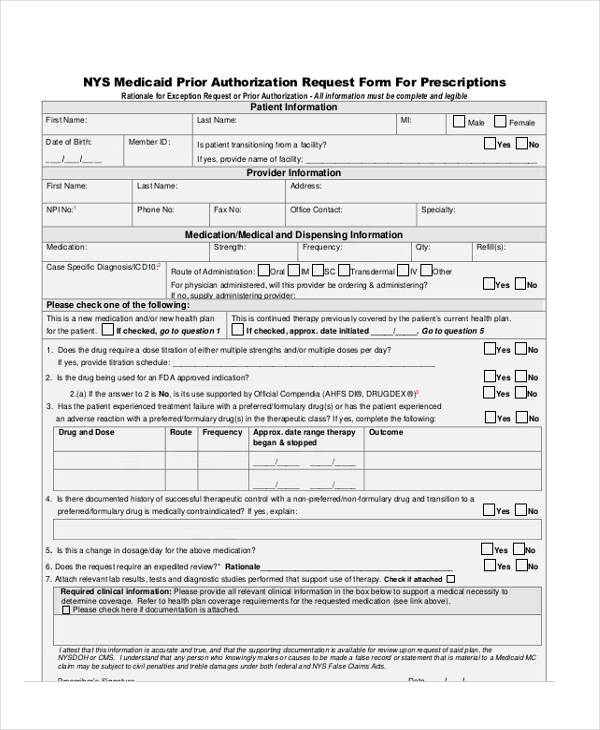
Hap Prior Authorization Form - Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Emergency room visits don’t require prior authorization. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. For inpatient hospital stays, your doctor will get prior authorization from hap.
Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. For inpatient hospital stays, your doctor will get prior authorization from hap. Emergency room visits don’t require prior authorization. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations.
Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. For inpatient hospital stays, your doctor will get prior authorization from hap. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Emergency room visits don’t require prior authorization.
Fillable Online Prior Authorization Criteria Form Fax Email Print
Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Emergency room visits don’t require prior authorization. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits..
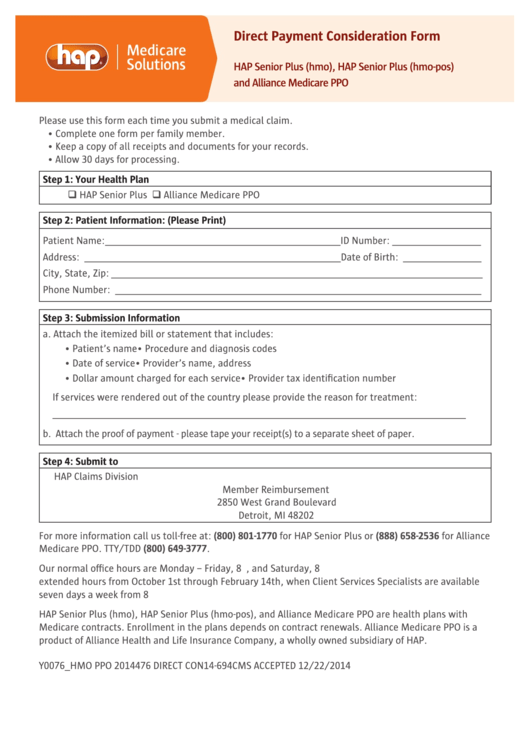
Hap Direct Payment Consideration Form printable pdf download
Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Emergency room visits don’t require prior authorization. Participating physicians and providers requesting authorization for medications can complete the appropriate form.
Fillable Online Hap Prior Authorization Form PDF Fill Out and Sign
Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Cms today unveiled a.
Efficient Ways to Handle Prior Authorization Process
For inpatient hospital stays, your doctor will get prior authorization from hap. Emergency room visits don’t require prior authorization. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations..
FREE 13+ Prior Authorization Forms in PDF MS Word
For inpatient hospital stays, your doctor will get prior authorization from hap. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Participating physicians and providers requesting authorization for.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. For inpatient hospital stays, your doctor will get prior authorization from hap. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Hap caresource™ evaluates prior authorization requests based on medical.
Medicare Update Prior Authorization Request Process for Certain
Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Emergency room visits don’t require prior authorization. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Participating physicians and providers requesting authorization for medications can complete the appropriate form below.
Fillable Online MIMEDP2339255 MI HAP Fillable Pharmacy Prior
Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. For inpatient hospital stays, your doctor will get prior authorization from hap. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Approved prior authorizations are contingent upon the eligibility of member at the.
20152024 HI Standardized Prescription Drug Prior Authorization Form
Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan..
Investment Thesis Reports — FCA Venture Partners
Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Emergency room visits don’t require prior authorization. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Prior authorization is a decision by the health insurer or plan that a.
Hap Caresource™ Evaluates Prior Authorization Requests Based On Medical Necessity, Medical Appropriateness And Benefit Limits.
Emergency room visits don’t require prior authorization. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. For inpatient hospital stays, your doctor will get prior authorization from hap.
Hap Empowered Health Plan, Inc., A Michigan Medicaid Health Plan, Is A Wholly Owned Subsidiary Of Health Alliance Plan Of Michigan.
Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations.