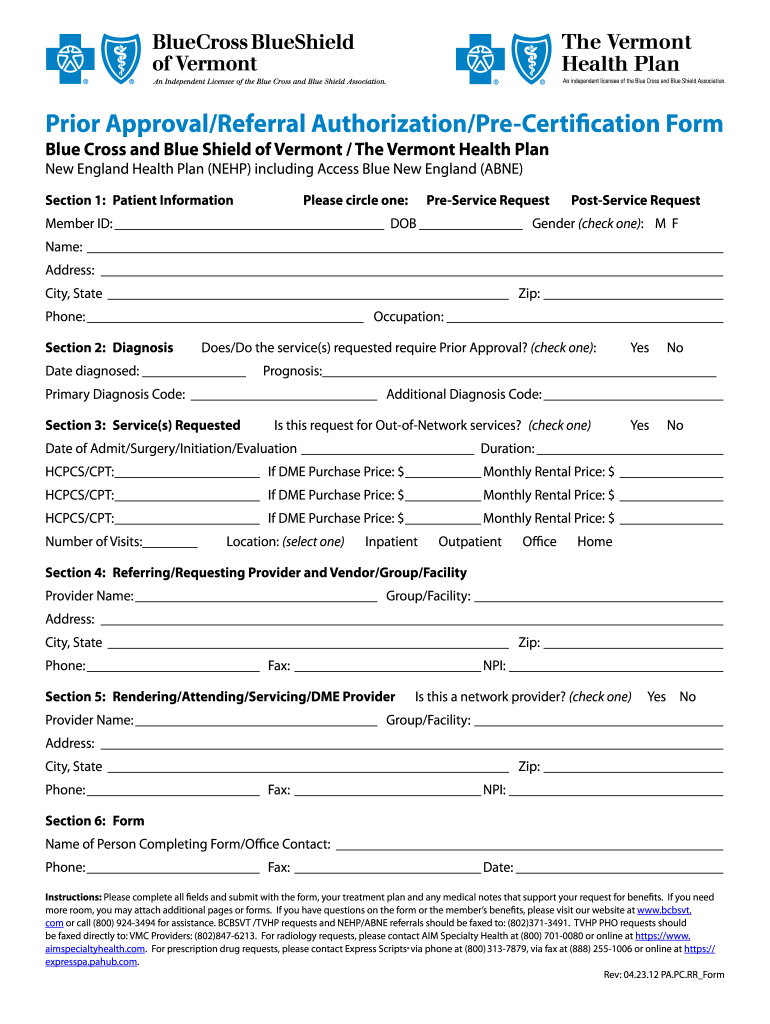
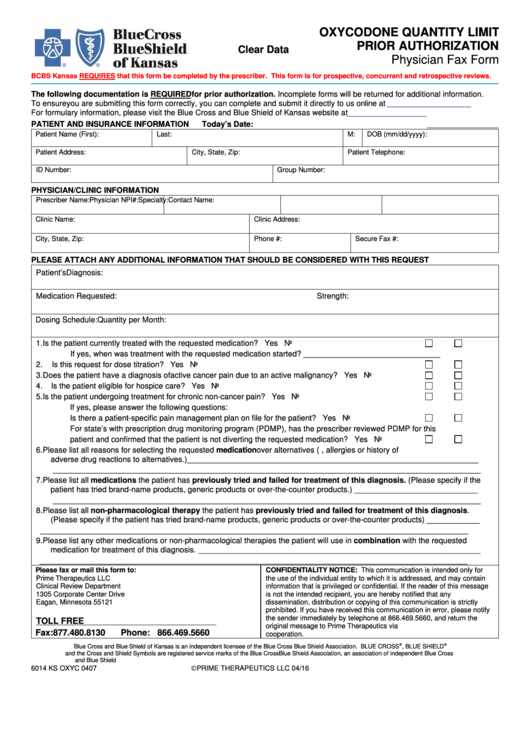
Blue Cross Blue Shield Pre Authorization Form
Blue Cross Blue Shield Pre Authorization Form - To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: This will determine if prior authorization will be obtained. Confirm if prior authorization is required using availity ® or your preferred vendor. There are different ways to initiate your request. Fax to the appropriate number: For prior authorization requests handled by bcbsil: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. Use blueapprovr sm to request prior authorization for some inpatient and/or outpatient, medical and surgical services and specialty pharmacy.
To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: For prior authorization requests handled by bcbsil: Fax to the appropriate number: There are different ways to initiate your request. Use blueapprovr sm to request prior authorization for some inpatient and/or outpatient, medical and surgical services and specialty pharmacy. This will determine if prior authorization will be obtained. Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. Confirm if prior authorization is required using availity ® or your preferred vendor.
To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. Use blueapprovr sm to request prior authorization for some inpatient and/or outpatient, medical and surgical services and specialty pharmacy. For prior authorization requests handled by bcbsil: This will determine if prior authorization will be obtained. There are different ways to initiate your request. Confirm if prior authorization is required using availity ® or your preferred vendor. Fax to the appropriate number:
Blue Cross Massachusetts Prior Authorization Forms Form Resume
There are different ways to initiate your request. This will determine if prior authorization will be obtained. For prior authorization requests handled by bcbsil: To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: Fax to the appropriate number:
CA Blue Shield C15390L 2020 Fill and Sign Printable Template Online
Fax to the appropriate number: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. For prior authorization requests handled by bcbsil: There are different ways to initiate your request. To request prior authorization, contact companion benefits alternatives (cba) using one of the below options:
Fillable Online Bcbs of minnesota prior authorization form Fax Email
For prior authorization requests handled by bcbsil: This will determine if prior authorization will be obtained. Fax to the appropriate number: Confirm if prior authorization is required using availity ® or your preferred vendor. There are different ways to initiate your request.
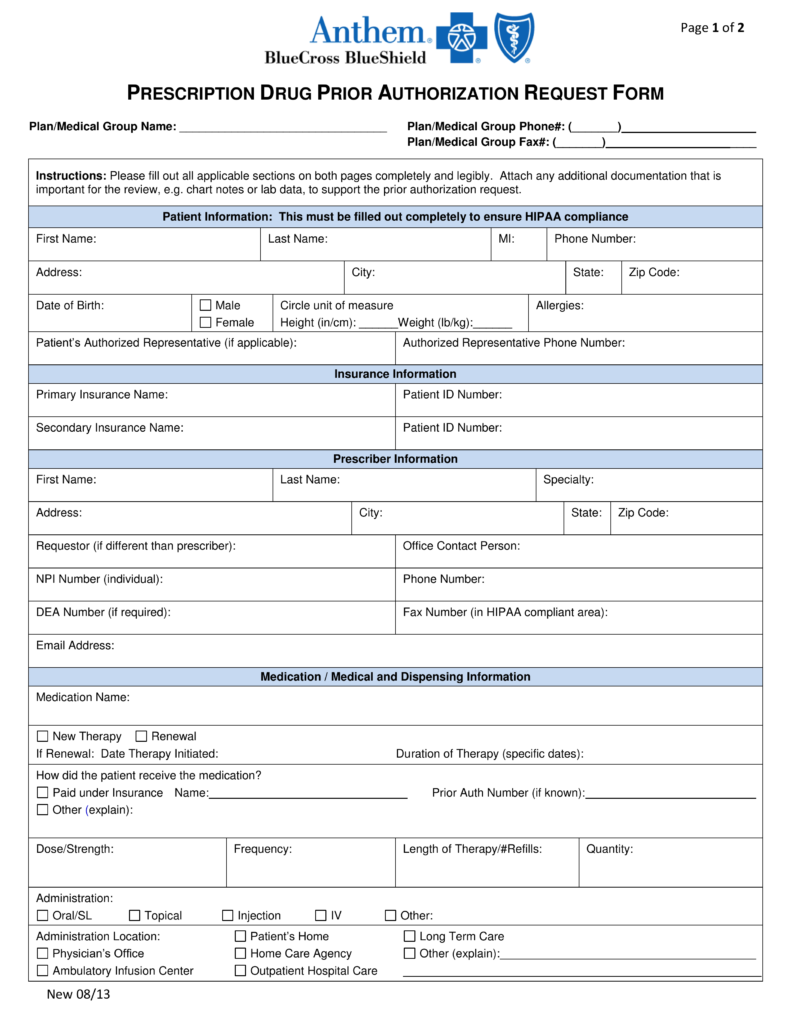
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained. There are different ways to initiate your request. Fax to the appropriate number: Use blueapprovr sm to request prior authorization for some inpatient and/or outpatient, medical and surgical services and specialty pharmacy.
Blue Cross Blue Shield Of Massachusetts Prior Authorization Form
This will determine if prior authorization will be obtained. To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: Fax to the appropriate number: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. Confirm if prior authorization is required using.
Wegovy Prior Authorization Form Blue Cross Blue Shield Form example
Confirm if prior authorization is required using availity ® or your preferred vendor. To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. For prior authorization requests handled by bcbsil: There.
Blue cross blue shield overseas claim form Fill out & sign online DocHub
This will determine if prior authorization will be obtained. To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: Use blueapprovr sm to request prior authorization for some inpatient and/or outpatient, medical and surgical services and specialty pharmacy. Fax to the appropriate number: For prior authorization requests handled by bcbsil:
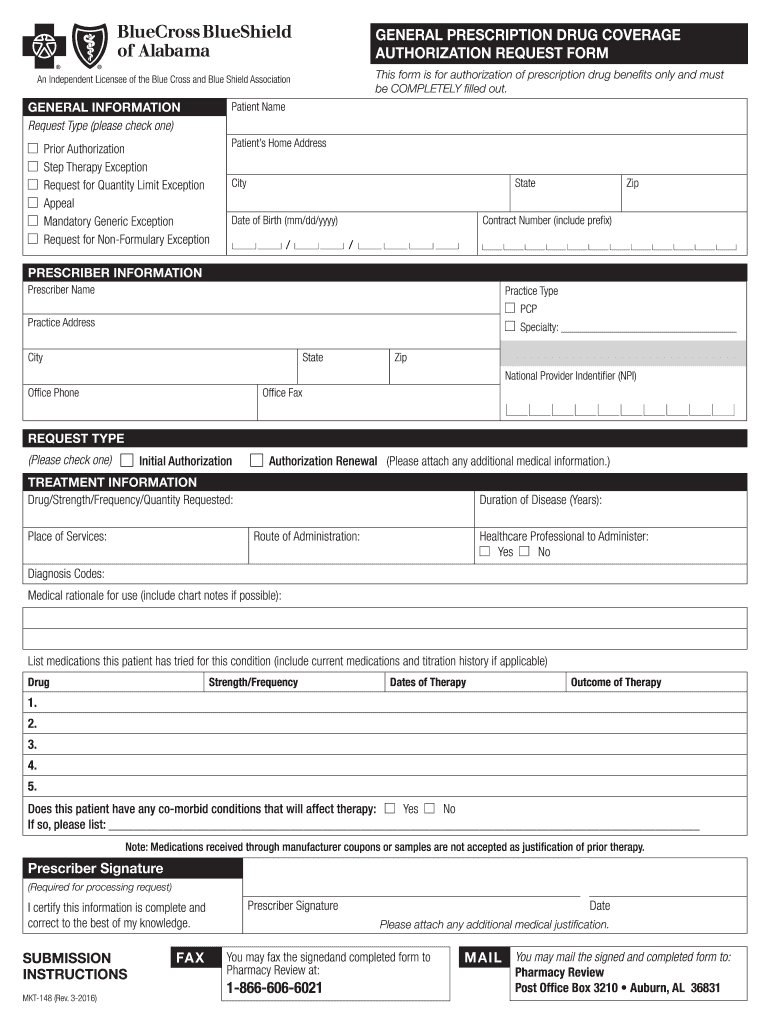
Blue Cross Blue Shield of Alabama Prior Authorization 20082024 Form
To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. There are different ways to initiate your request. This will determine if prior authorization will be obtained. Confirm if prior authorization.
Free Anthem (Blue Cross Blue Shield) Prior (Rx) Authorization Form
For prior authorization requests handled by bcbsil: There are different ways to initiate your request. Confirm if prior authorization is required using availity ® or your preferred vendor. Fax to the appropriate number: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a.
Blue Shield Highmark Bcbs Prior Auth Form
Confirm if prior authorization is required using availity ® or your preferred vendor. For prior authorization requests handled by bcbsil: This will determine if prior authorization will be obtained. Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. There are different ways to initiate your.
Confirm If Prior Authorization Is Required Using Availity ® Or Your Preferred Vendor.
For prior authorization requests handled by bcbsil: Fax to the appropriate number: Ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a. Use blueapprovr sm to request prior authorization for some inpatient and/or outpatient, medical and surgical services and specialty pharmacy.
This Will Determine If Prior Authorization Will Be Obtained.
To request prior authorization, contact companion benefits alternatives (cba) using one of the below options: There are different ways to initiate your request.